Women’s Health or pelvic health physiotherapy is not included in the nice guidelines for endometriosis, however it is included in the nice guidelines for chronic pelvic pain.
Physiotherapy is not part of the care offered to most women who have been diagnosed with or have symptoms of endometriosis, either before or after surgery. Laparoscopic excision of endometrial lesions is the gold standard treatment, performed by a gynaecologist who has specialist training in this surgery.
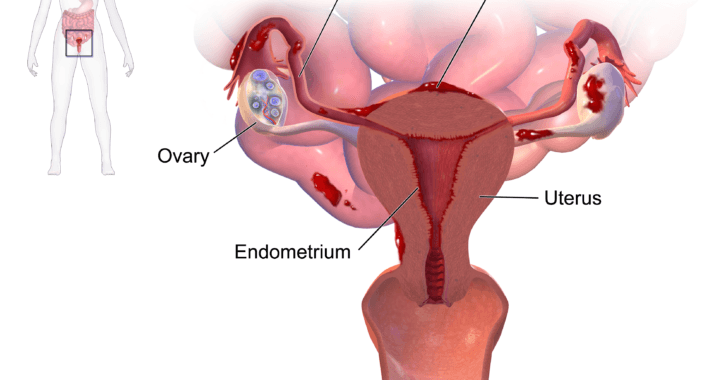
With 1:10 women diagnosed with endo it is surprising that on average the diagnosis takes between 7 and 10 years. Endo is as common as diabetes and asthma and yet is not as well understood even though women have been suffering for years.
This needs to change and hopefully by educating you as to how physio can help you will be more informed and can therefore spread the word!
Who presents to my clinic?
The women who present to my clinic rarely come specifically with a diagnosis of endometriosis. They come with symptoms such as pain during sex, low back pain, constipation or bladder and bowel symptoms. Interstitial Cystitis is a common ‘evil twin’ of endo and is a very specific issue concerning the bladder lining. Painful Bladder Syndrome is more of a global name for pain around the bladder.
These women have usually had their pain and dysfunction for some time hoping that their symptoms would improve or disappear.
It is only when questioned about their periods that they may disclose that they have endo or have been having issues with their cycle since their teenage years. Most of the women that I see in this situation have issues far beyond that of a diagnosis of endometriosis. They are also dealing with fatigue, stress and anxiety, infertility, issues at work and within their relationships.
At this point it is noticeable that it is not just the body that needs help but also the mind. Pelvic health physiotherapy should be a holistic, integrative treatment which involves education, hands on treatment and support.
How can physiotherapy help?
- We can sit and listen to your whole story – the one that you’ve been trying to tell since your periods began. We hold space so you can tell us your worries and concerns for your future. We never judge you when you tell us how you really feel, the feelings that may be hard to explain to a friend or family member who doesn’t know what you’re dealing with.
- We will ask you what investigations, treatments and surgeries you have undergone. Maybe stress is playing a part in ramping up your pain and symptoms – this is something that many people don’t associate with their pain.
- We will ask questions about your home life, work life, sex life, menstrual cycle, nutrition, hydration, fertility – we like to gather as much information as possible to help us formulate a plan of action with you. Treatment/management of your condition should never be ‘done’ to you, you are an integral part of your treatment and must consent and agree.
Pain education
- This is an important part of your treatment. Some of you may have already been to pain clinic and this can lead to variable experiences. Much of the time pain clinic will consist of medication being prescribed to help with your pain and symptoms. Depending on how pain is described to you, you may be left feeling that you are being told that the pain is in your head. This can increase your feelings of helplessness anxiety and stress.
- Pain is a very complex subject. However, there are ways of simplifying the explanation so that it is more easily understood.
- For example, one day you went for a poo and having that poo caused a lot of pain. The next day you start having the sensation of needing a poo and immediately you start feeling pain even though you are not yet sat on the toilet. You have remembered your bad experience from the day before and therefore your brain is out putting pain signals even before anything has happened.
- The way our pain mechanisms work is useful at times to prevent us injuring ourselves. For example, we remember that when we put our hand in the fire it caused us pain and injury. Therefore to prevent us injuring ourselves further we have learned not to put our hand in the fire.
- Pain is a decision of the brain and is affected by how much threat you are under. Pain can be affected by the situation you are in, the environment around you, language that has been used by health professionals or how safe you feel. After considering your situation your brain will decide on a pain output and this is what you will feel.
- Pain does not equal tissue damage. We will always feel pain before tissue damage occurs. A buffer zone is created to prevent us injuring ourselves. This buffer zone can be increased and decreased by factors such as mood, sleep, nutrition, thoughts, expectations and beliefs.
- For this reason we must consider all aspects of your history and lifestyle when we are treating you.
Breathing
- Teaching you how to use your breath is usually the first intervention which we provide in your treatment.
- Pain can lead to an altered breathing pattern which in itself stresses the body as we are not getting enough oxygen into our lungs. Learning to breathe optimally will have benefits which are far reaching.
- The vagus nerve which brings peace and relaxation to our nervous system can be stimulated by breathing low and wide into our lungs. By exhaling for twice as long as our inhale we can really ramp up and tonify this nerve, which is involved in brain, gut and heart health to name a few. What it can also do is help down regulate our nervous system and bring us out of ‘fight or flight’ into ‘rest and restore’.
Exercise and movement
- Motion is lotion and when we are in pain, or suffering with heavy period, movement is the last thing on our minds. It might be that moving in a particular direction increases your pain and feels that it is pulling through your abdomen or even the whole side of your body. At this point you want to curl up in a ball, and that’s fine! Movement however can mobilise tissues around your organs as well as the organs themselves.
- Research shows the exercise and movement especially outside in the daylight can help your mental health. Vitamin D, which is made by the interaction of day light on our skin, is important for bone and tissue health.
- Many women with endo have undergone a hysterectomy due to comorbidities such as adenomyosis and fibroids. If the ovaries have been removed as well as the uterus, then the lack of oestrogen within the body can have an effect on bone health, brain health and heart health.
- It is important to find a way that you can move and be active and as physiotherapist we can give advice and exercise programmes designed around your symptoms.
- Yoga and Pilates are two forms of exercise that may be a good place to start. These integrate balance, strength, mindfulness and flexibility.
Here is a link to a stretch and breathing video I recorded https://youtu.be/_YAj_JM_IRI
Hands on treatment
- Physiotherapists are specialists in hands-on manual therapy. We are all trained to use our hands to assess and treat. Some of us will have also trained in more specialised techniques.
- We can work on muscles, nerves and joints, scar tissue, trigger points and also your viscera (internal organs) with extra training.
- This can help to down regulate your nervous system as well as increasing the mobility of the external and internal tissues.
Pelvic floor release
- Many women with abdominal and pelvic pain will present with an overactive pelvic floor.
- Research shows that the pelvic floor will increase in tension when we are in a stressful situation. Being in pain and feeling under threat will cause the pelvic floor to tighten and not necessarily release.
- An important part of physiotherapy management is teaching you to relax and release or down train your pelvic floor. This can be done through visualization and guided imagery, breathing and stretches.
- As pelvic health physiotherapists, we are trained to do internal release work on the pelvic floor. This involves an internal examination of the pelvic floor and treatment as found necessary.
- We can also advise and educate on the use of dilators and wands for continued home treatment.
If you have any questions or concerns about your pelvic health please contact your GP, gynaecologist or pelvic health physiotherapist.
For support visit Endometriosis UK.